M-F 9am - 8pm EST
Impact of Chronic Conditions on Mobility
As we age, the cumulative effects of chronic conditions can profoundly influence an individual's mobility, leading to a cascade of challenges that hinder the ability to move freely and comfortably. For older adults, these conditions often accelerate the natural decline in physical function, necessitating significant adjustments to lifestyle, daily routines, and overall independence.
Losing the ability to move with ease can lead to a sense of helplessness and isolation, as routine activities, like walking, climbing stairs, or even getting dressed, become increasingly difficult. What may begin as minor discomfort or inconvenience can quickly evolve into more substantial mobility issues, as age-related changes, combined with the long-term impact of chronic conditions, compound over time.
The impact of chronic conditions on mobility in older adults goes far beyond physical limitations. It also significantly influences mental health, emotional well-being, independence, and overall quality of life. Here’s a closer look at how chronic conditions, often exacerbated by the aging process, impact mobility:
Joint and Musculoskeletal Disorders
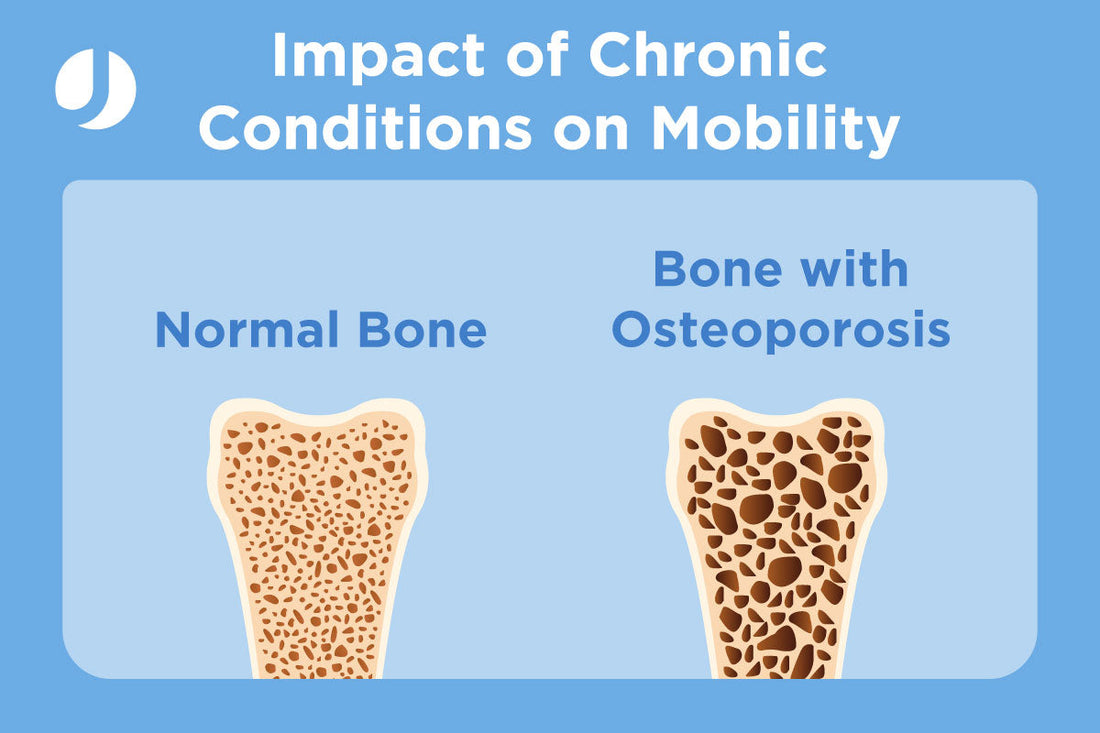
Osteoporosis:
A condition where bones become weak and brittle due to a decrease in bone density.

Impact on Mobility from Osteoporosis:
- Increased risk of fractures, especially in the spine, hips, and wrists, which can limit movement.
- Pain and deformities (e.g., stooped posture or kyphosis) from vertebral fractures.
- Reduced ability to engage in weight-bearing activities, leading to weakness and muscle atrophy.
Management: Medications to strengthen bones, weight-bearing exercises, fall prevention strategies.
Osteoarthritis (OA)
The gradual breakdown of cartilage in the joints leads to bone-on-bone friction, causing pain, swelling, and reduced joint function.
Impact on Mobility from Osteoarthritis:
- Pain and stiffness, especially after long periods of rest or during weight-bearing activities like walking or climbing stairs.
- Decreased flexibility and range of motion in affected joints.
- Joint instability, which can lead to difficulty walking or performing activities like bending or squatting.
Management: Exercise, weight management, pain relief medications, physical therapy, and in severe cases, joint replacement surgery.
Rheumatoid Arthritis (RA)
An autoimmune disease where the body’s immune system attacks the synovial lining of the joints, causing inflammation and damage.
Impact on Mobility from Rheumatoid Arthritis:
- Chronic pain, especially in the morning, and swelling in the joints.
- Deformation of the joints, particularly in the hands, wrists, and knees, leading to functional limitations.
- Difficulty performing fine motor tasks and walking due to joint deformities and pain.
Management: Disease-modifying antirheumatic drugs (DMARDs), biologics, pain management, and physical therapy to preserve joint function.
Cardiovascular Diseases
Arrhythmia
Irregular heart rhythms can reduce cardiac output, leading to insufficient blood flow to muscles during activity.
Impact on Mobility from Arrhythmia:
- Fatigue and dizziness, which may limit the ability to walk or stand for extended periods.
- Risk of fainting during exertion.
Management: Medications, lifestyle modifications, and sometimes pacemakers or defibrillators.

Atrial Fibrillation (AFib)
Irregular and often rapid heart rate reduces the heart's efficiency in pumping blood.
Impact on Mobility from Atrial Fibrillation:
- Fatigue, weakness, and reduced physical capacity during exertion.
- Risk of stroke, which can lead to long-term mobility challenges.
Management: Medications to control heart rate, prevent blood clots, and lifestyle changes.
Chronic Venous Insufficiency (CVI)
Damaged veins in the legs impair blood flow back to the heart, leading to pooling of blood in the lower extremities.
Impact on Mobility from Chronic Venous Insufficiency:
- Leg pain, swelling, and heaviness that worsen with prolonged standing or walking.
- Skin changes and ulcers may limit activity.
Management: Compression therapy, physical activity, and, in some cases, surgical interventions.
Coronary Artery Disease (CAD)
Reduced blood flow to the heart muscle due to plaque buildup in the coronary arteries limits the heart's ability to meet increased oxygen demands during physical activity.
Impact on Mobility from Coronary Artery Disease:
- Chest pain (angina) during exertion can discourage physical activity.
- Reduced stamina and endurance.
- Fear of triggering a cardiac event (e.g., heart attack) may lead to reduced activity levels.
Management: Medications to improve heart function, lifestyle changes, and interventions like stenting or bypass surgery.
Heart Failure
The heart’s reduced ability to pump blood effectively leads to inadequate oxygen and nutrient delivery to muscles.
Impact on Mobility from Heart Failure:
- Chronic fatigue and shortness of breath during physical activity.
- Swelling in the legs and feet (edema), making walking uncomfortable.
- Reduced physical endurance and difficulty performing daily tasks.
Management: Lifestyle changes, medications, and cardiac rehabilitation to improve heart function and physical capacity.
Hypertension
Chronic high blood pressure strains the heart and damages blood vessels, affecting circulation.
Impact on Mobility from Hypertension:
- Reduced endurance and stamina.
- Increased risk of complications such as stroke or PAD, which further impair mobility.
Management: Blood pressure control through diet, exercise, and medications.
Peripheral Artery Disease (PAD)
Narrowed or blocked arteries in the legs reduce blood flow to muscles during activity.
Impact on Mobility from Peripheral Artery Disease:
- Leg pain or cramping (claudication) during walking or climbing stairs.
- Reduced walking speed and distance.
- Weakness and discomfort, leading to avoidance of physical activity.
Management: Supervised exercise programs, medications to improve circulation, and surgical interventions like angioplasty in severe cases.
Stroke
Interruption of blood flow to the brain causes neurological impairments, often affecting motor function and coordination.
Impact on Mobility from Stroke:
- Partial or complete paralysis, often on one side of the body (hemiplegia).
- Difficulty with balance, coordination, and walking.
- Increased reliance on assistive devices such as canes or wheelchairs.
Management: Physical and occupational therapy to regain strength and mobility, as well as secondary prevention to reduce future stroke risk.
Neurological Disorders
Dementia (e.g., Alzheimer’s Disease)
Progressive brain degeneration affects cognition, motor planning, and coordination.
Impact on Mobility from Dementia:
- Difficulty navigating spaces and coordinating movements.
- Increased risk of falls due to balance problems and slower reaction times.
- Gait disturbances, often characterized as a "hesitant" or "wandering" gait.
Management: Fall prevention strategies, structured routines, and physical activity.
Multiple Sclerosis (MS)
Immune-mediated damage to the myelin sheath in the central nervous system disrupts nerve signals.
Impact on Mobility from Multiple Sclerosis:
- Muscle weakness, spasticity, and coordination issues.
- Fatigue and balance problems.
- Difficulty walking (gait abnormalities) and increased fall risk.
- Severe cases may require mobility aids like wheelchairs or walkers.
Management: Physical therapy, assistive devices, and medications to manage spasticity and fatigue.
Parkinson’s Disease
Degeneration of dopamine-producing neurons in the brain leads to impaired motor control.
Impact on Mobility from Parkinson’s Disease:
- Tremors, stiffness, and slowness of movement (bradykinesia).
- Difficulty initiating movements, leading to a "freezing" sensation.
- Postural instability increases the risk of falls.
- Shuffling gait and reduced arm swing during walking.
Management: Medications like levodopa, physical therapy, and gait training.
Peripheral Neuropathy
Damage to peripheral nerves affects sensation and motor function.
Impact on Mobility from Peripheral Neuropathy:
- Numbness, tingling, or pain, particularly in the hands and feet.
- Muscle weakness and difficulty with balance or coordination.
- Increased risk of falls due to lack of proprioception (awareness of body position).
Management: Addressing the underlying cause (e.g., diabetes), physical therapy, and supportive footwear.
Other Chronic Conditions
Diabetes
- Effect on Mobility: Diabetes can lead to complications such as peripheral neuropathy (nerve damage), foot ulcers, and poor circulation. These conditions can cause pain, numbness, or a lack of sensation in the feet, affecting balance and walking.
- Key Challenges: Increased risk of falls, difficulty in wound healing (leading to potential amputations), and reduced physical activity due to discomfort or fear of injury.
Management: Blood sugar control, regular foot care, wearing proper footwear, and engaging in low-impact activities like tai chi or yoga to improve balance.
Obesity
- Effect on Mobility: Excess body weight puts added stress on weight-bearing joints (e.g., hips, knees), leading to faster joint degeneration and pain. Obesity is also associated with reduced stamina and balance.
- Key Challenges: Increased risk of osteoarthritis, difficulty in performing daily activities, and higher likelihood of developing other conditions (e.g., diabetes, cardiovascular diseases) that further impair mobility.
Management: Weight loss through diet and exercise, participation in physical therapy, and the use of assistive devices to reduce joint strain.
The impact of chronic conditions on mobility is complex and multifaceted. These conditions often intertwine, with one exacerbating the effects of another, leading to a vicious cycle of decline. However, with early intervention, proper management, and targeted rehabilitation strategies, individuals can maintain or even improve their mobility, enhancing their independence and quality of life.
Through a combination of medical treatment, physical therapy, and lifestyle adjustments, individuals facing mobility challenges can still lead active, fulfilling lives despite their chronic conditions.
References
Anne B Newman, The Epidemiology and Societal Impact of Aging-Related Functional Limitations: A Looming Public Health Crisis, The Journals of Gerontology: Series A, Volume 78, Issue Supplement_1, June 2023, Pages 4–7, https://doi.org/10.1093/gerona/glad021
Wilder CS. Chronic Conditions and limitations of Activity and Mobility, United States - July 1965-June 1967. Vital Health Stat 10. 1971 Jan;(61):1-75. PMID: 25198557.
Davis, James et al. “Relation of incident chronic disease with changes in muscle function, mobility, and self-reported health: Results from the Health and Retirement Study.” PLOS global public health vol. 2,9 e0000283. 8 Sep. 2022, doi:10.1371/journal.pgph.0000283
https://acornhcs.com/arthritis-a-silent-thief-of-mobility-in-the-elderly/
https://www.lohmedical.com/en/solutions/osteoporosis-and-mobility-issues
https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2022.856260/full
https://strokefoundation.org.au/what-we-do/for-survivors-and-carers/after-stroke-factsheets/mobility-and-exercise-after-stroke-fact-sheet
https://www.parkinson.org/understanding-parkinsons/movement-symptoms/trouble-moving
https://www.lohmedical.com/en/solutions/alzheimers-disease-and-mobility-issues
https://www.tandfonline.com/doi/full/10.1586/erp.10.34
https://www.lohmedical.com/en/solutions/diabetes-and-mobility






